We use cookies on this website to enhance your user experience. Please read our cookie policy for additional information and a complete overview. We will only use cookies if you consent by clicking on “Accept all cookies”. You can always manage your preferences via the settings of your browser. Please note that certain media will only be available if you have accepted the applicable cookies.
Towards standardized EEG source imaging in the presurgical work-up
of patients with epilepsy
Ghent, 22/8/2017. In today’s presurgical work-up, the patient is investigated with different neuroimaging techniques to identify the epileptogenic zone. The techniques that are included differ from center to center. Most centers perform video-EEG monitoring, MRI and interictal PET, but do not perform EEG source imaging to localize the epileptogenic zone. In this post, we discuss the added value of the different techniques and the advantages of including EEG source localization during phase 1 in your presurgical work-up.

Worldwide there are more than 70 million people with epilepsy. Approximately 1/3 of them can not obtain adequate control of seizures using anti-epileptic drugs. These patients have pharmaco-resistant epilepsy. In this case surgical resection of the epileptogenic zone (EZ) – the area in the brain causing the epilepsy – may be the best treatment option. An extensive presurgical work-up is required to localize the EZ to investigate whether the patient is eligible for epilepsy surgery and which region should be removed.
This work-up consists of several diagnostic steps. In the first phase the three cornerstone investigations are magnetic resonance imaging (MRI), long-term electro-encephalography (EEG) video monitoring and neuropsychological testing. MRI is used to visualize structural abnormalities in the brain while EEG records the electrical activity of the brain to detect epileptic discharges. In many patients, a second phase is required, using other investigations such as positron emission tomography (PET), single photon emission tomography (SPECT), functional MRI, Wada-test and magneto-encephalography (MEG) to further delineate the epileptogenic zone. When necessary, intracranial EEG can be recorded in a third step to exactly define the EZ and perform invasive functional mapping of eloquent tissue. Although this work-up is used in many centers, there are only few recommendations on the use and specification of these techniques.
The European Union-funded E-PILEPSY project has conducted a study to gain insight into the differences of this presurgical diagnostic workup between 24 European centers (1). They have concluded that there is a large variation in the usage of imaging techniques between the different epilepsy surgery centers.
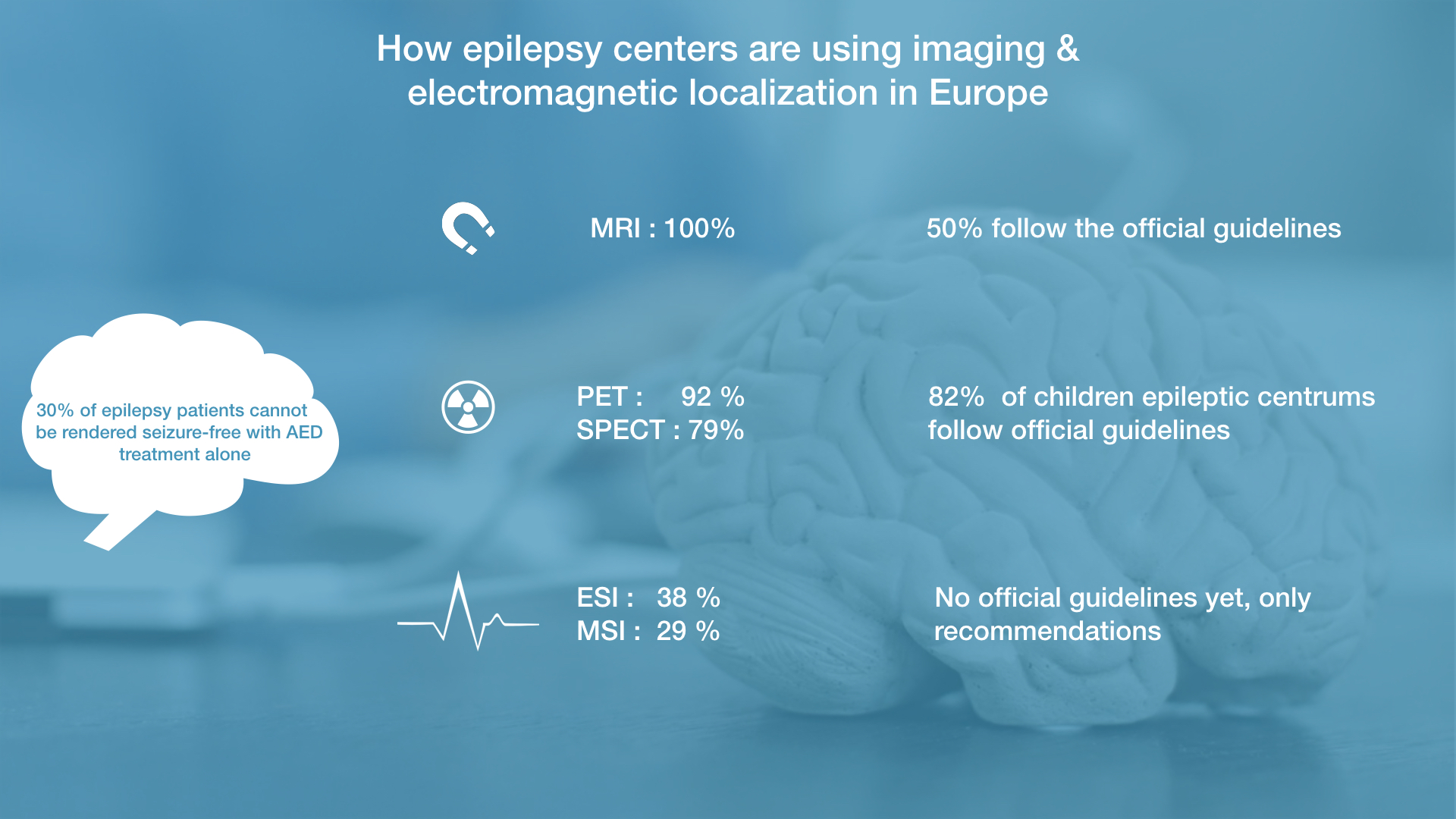
More into detail, MRI is used in every center for presurgical work-up but only half of them follow the recommended guidelines. Interictal PET is available in 92% of the centers, while ictal SPECT is less widely available (79%). This lower usage of SPECT is probably due to a higher workload, the cost of seizure monitoring and the necessity to capture a seizure. 82% of the pediatric epilepsy centers have at least one of these two nuclear imaging modalities, following the recommended guidelines.
Less commonly used are the electromagnetic source imaging techniques, magnetic source imaging (29%) and electroencephalography source imaging (ESI; 38%). The low usage for trustworthy ESI is due to the need of required technical expertise together with specialized software. Moreover, ESI is usually not applied on typical long-term EEG recordings but on additional EEG recordings for source localization which increases the costs. Another reason is that there are no recommended guidelines yet, only some recommendations, which doesn’t promote the usage of this technique.
It is surprising that ESI is only used in the minority of centers, as its accuracy has been demonstrated within the presurgical work-up (2). A recent prospective study has shown that ESI can more accurately estimate the EZ than other techniques for difficult cases in epilepsy surgery such as MRI-negative or frontal lobe epilepsies(3).
As a consequence, Epilog believes that ESI should be used in the first phase of the presurgical work-up for several reasons. First, a higher sensitivity (80%) and specificity (75%) than PET, SPECT or MRI has been demonstrated when using state-of-the-art techniques and long-term EEG data (4).
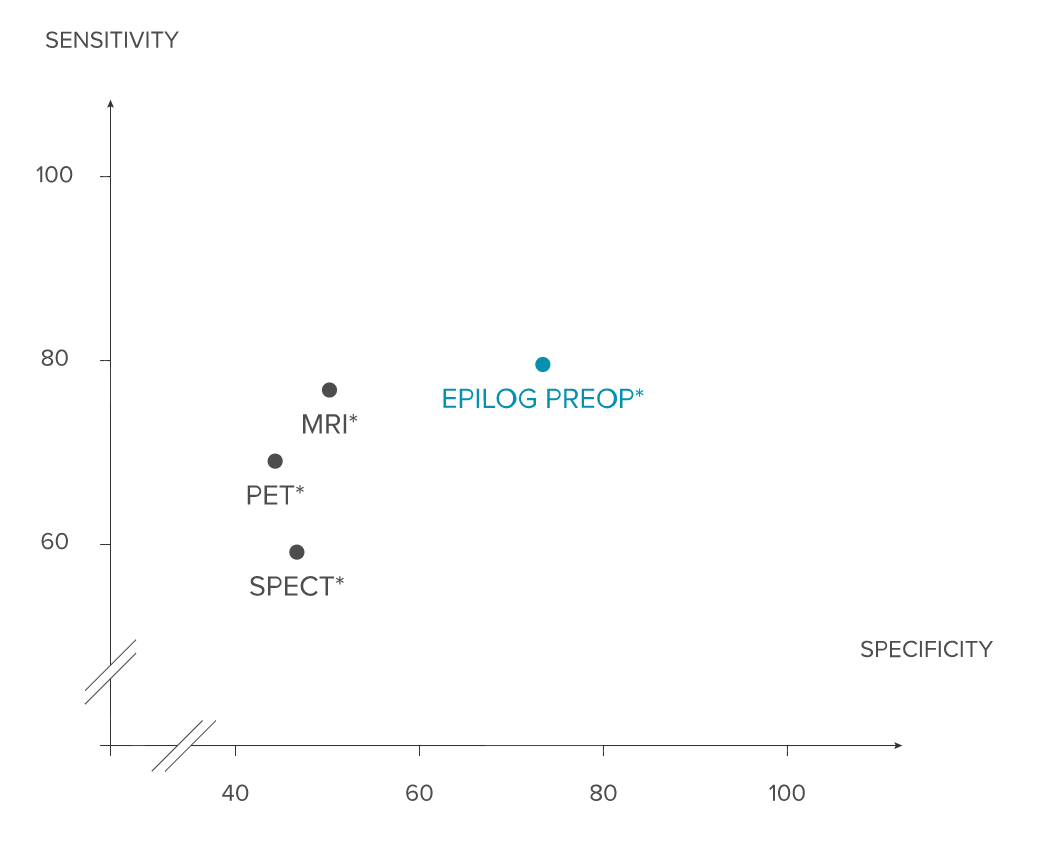
Second, ESI provides functional imaging of the epileptic activity on a sub-lobar level. Third, as the long-term EEG data is almost always available during the first phase of the presurgical work-up for refractory epilepsy, it should be used to its full extent when facing such a clinically challenging problem.
“Epilog is convinced that epilepsy centers should move beyond pure visual interpretation of long-term EEG in Phase 1 of the presurgical work-up.”
To stimulate the use of source localization in the clinical work-up, Epilog provides state-of-the-art ESI as a service solution to hospitals. For each patient, a standardized report depicting the detected spikes and their 3D localization in the brain based on a 6-layer model is made available for the treating neurologist in only a couple of minutes.
For more information, join our Epilog Symposium about Imaging Trends in Epilepsy Imaging on the 22th of September in Ghent, Belgium.
(1) Mouthaam et al. Current use of imaging and electromagnetic source localization procedures in epilepsy surgery centers across Europe (2016). Epilepsia 57,5, 770-776 (link)
(2) Brodbeck et al. Electroencephalographic source imaging: a prospective study of 152 operated epileptic patients (2011) ;134:2887–2897. (link)
(3) Abdallah et al. Localizing value of electrical source imaging: frontal lobe, malformations of cortical development and negative MRI related epilepsies are the best candidates (2017). NeuroImage Clinical (link)
(4) Van Mierlo et al. Automated long-term EEG analysis to localize the epileptogenic zone (2017). Epilepsia Open (link)

